A day after Vice President Mike Pence assured Americans that lab tests for coronavirus would be covered by private and government health insurance, that promise appears to be less than airtight.
The bottom line: Medicare, Medicaid, and “Obamacare” insurance plans will cover the tests, officials said Thursday. Major insurers also said they will cover such tests. But people with employer-provided insurance should check with their plan because copays and deductibles may apply. State health departments will test for free.
“It’s a common type of test, just like you get a swab for strep throat,” Seema Verma, head of the federal Centers for Medicare and Medicaid Services, told reporters on Capitol Hill. “I think private insurance companies, it does depend on coverage. But like I said, this is something that is commonly covered.”
Doctors and insurers stress that patients potentially exposed to coronavirus should not avoid getting tested because of concerns about potential costs.
The board of directors of an industry group that represents big insurance companies said Thursday that member plans will cover tests ordered by a doctor. “We will take action to ease network, referral, and prior authorization requirements and/or waive patient cost sharing,” America’s Health Insurance Plans said in a statement.
Translation: Call your insurance plan to see what particular steps it’s taking and whether you qualify for no-cost testing.
In Washington state, where at least 11 people have died, Insurance Commissioner Mike Kreidler moved to dispel doubts Thursday by ordering insurers in the state not to charge copays or deductibles to people who require coronavirus tests. The directive applies only to plans regulated by the state.
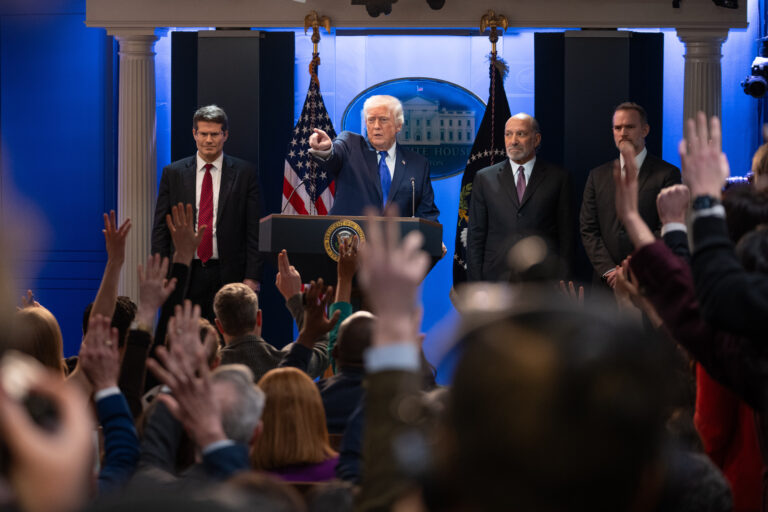
On Wednesday, Pence made what’s now looking like a work-in-progress seem like a done deal.
“With regard to the cost, let me be very clear,” Pence said at a White House briefing. The Health and Human Services Department “has designated the coronavirus test as an essential health benefit. That means by definition, it’s covered in the private health insurance of every American as well as covered by Medicare and Medicaid.”
Some independent experts were flummoxed, uncertain that the government has the authority to order blanket coverage of a medical service.
“I’m not sure what he means,” said Karen Pollitz of the nonpartisan Kaiser Family Foundation. “I can’t point to anything that would back that up.”
“Essential health benefits” is a term used in the Affordable Care Act to describe broad categories of care. Under the health law, preventive services have to be covered at no cost to the patient. But that designation requires a formal evaluation by an expert task force, and there’s no indication that has happened.
And the coronavirus test might be classified as a diagnostic test, not a preventive service. Usually, patients pay some of the cost for diagnostic tests, through copays and deductibles.
It’s unlikely that a patient will receive only one test for coronavirus. A doctor also might order a chest X-ray or tests for bacterial pneumonia or the flu, also respiratory diseases, depending on the patient’s symptoms.
Administration officials say coronavirus tests should be widely available in the next few days, and Verma said the government wants the broadest possible access. Responding to a question about concerns, she said, “We’re going to continue to look at that, that if it becomes an issue, I would say that’s something we want to make sure people have access to tests.”
With costs remaining an unresolved issue, Pollitz points out that the annual deductible for an employee covered by workplace insurance averages $1,655, and double that for families. Most deductibles reset every January, and consumers generally don’t satisfy theirs until May or later. Deductibles are higher for individual insurance plans.
About half of all insured adults in the United States worry about affording their deductible, according to a recent poll from the Kaiser Foundation.
Research shows that people with deductible worries don’t just avoid wasteful or unnecessary care, said Sabrina Corlette, co-director of Georgetown University’s Center on Health Insurance Reforms. “They’re actually not getting care they should be getting,” she said.
Plus there are an estimated 28 million uninsured people in the United States.
The American Academy of Family Physicians says uninsured people should contact their local health department or a community health center for help. Call first, in case officials need to prepare for a visit from someone who may have the virus.
Insured patients who are worried about bills should contact their doctor’s office or their insurer. They may be able to connect patients with a nurse or arrange a telemedicine visit to help decide whether an office visit is even needed.
Insurers also may be able to lay out all options for care and what a visit may cost according to a patient’s coverage.
Insurers may also ease requirements such as a large deductible payment for some care.
“Our first priority is to ensure our members have access to the diagnostic and treatment care they need, and we are continuing to work with our customers and policy-makers on this public health challenge,” said Eric Hausman, a spokesman for the insurer UnitedHealthcare.
(AP)










One Response
Gaslighting. If you can’t afford the tests you won’t be able to afford the “costs” either. With our lack of low-cost medical care and lack of sick days for hourly workers, we are setting ourselves up for a real US epidemic.