We are a community that cares. When a child is sick, we seek the best doctors. When someone needs help, we show up. And Baruch Hashem, when it comes to mental health, we’ve come a long way. People are going to therapy. We’re talking more openly. The stigma is breaking.
But something isn’t adding up.
People are spending years in therapy — and still suffering.
The anxiety is still there.
The depression hasn’t lifted.
The trauma still haunts.
Relationships remain broken.
And families feel like they’re drowning.
Too many people go to therapy hoping for healing — and walk away with little more than “processing,” “insight,” or “support.” While that can be meaningful, it’s often not enough. Not when someone is truly struggling. Not when they need to get better.
And here’s what most people don’t realize:
There are treatments that work.
Not just in theory. Not just emotionally. But practically. Clinically. Measurably.
These are called evidence-based therapies — approaches tested through decades of research, refined through thousands of clinical cases, and shown to consistently reduce symptoms. For real.
Here’s what that looks like:
- CBT (Cognitive Behavioral Therapy) — 12 to 20 sessions for anxiety, depression, and more
- ERP (Exposure and Response Prevention) — 12 to 20 sessions for OCD
- DBT (Dialectical Behavior Therapy) — 6 to 12 months for emotion dysregulation and self-destructive behavior
- PCIT (Parent-Child Interaction Therapy) or PMT (Parent Management Training) — 12 to 20 sessions for childhood behavior challenges like ADHD
- CPT and PE — 8 to 15 sessions for trauma and PTSD
Compare that to therapy that drags on for years, with no clear direction, and no measurable change.
(And think of the savings! Therapy just isn’t so expensive anymore when you are talking about these timelines.)
When you choose evidence-based therapy, you’re not just paying to be heard.
You’re investing in progress.
Let’s be clear. Evidence-based therapy isn’t cold or rigid. It’s not robotic. And it’s definitely not shallow. It doesn’t ignore emotions — it uses them. It doesn’t avoid the past — it teaches you how to stop being controlled by it. These treatments are structured, collaborative, and deeply respectful. And they’re designed to work.
CBT doesn’t just explain why you feel stuck. It helps you get unstuck.
DBT doesn’t just teach you skills. It helps you use them when it counts.
ERP doesn’t help you avoid your fears. It helps you face them and win.
PCIT doesn’t just calm your kid. It transforms your parenting.
And trauma therapy isn’t endless. It’s targeted. It’s focused. And it brings relief.
So why haven’t more people in our community heard of these approaches?
It’s not because therapists don’t care. It’s often because they weren’t trained in them. Many talented, well-meaning therapists never learned how to use these treatments. That’s not their fault — but it’s a gap we need to talk about. Because when people are in pain, they deserve more than good intentions. They deserve tools that are proven to help.
This isn’t about criticizing therapists. It’s about protecting clients.
It’s about saying: if you’re suffering, you deserve to know what works.
And if you’re investing time, money, and hope in therapy, you deserve to understand what you’re getting.
Every person in therapy should feel empowered to ask:
- What treatment are we doing?
- What is it meant to treat?
- What does the research say? Is this treatment proven by tens of clinical trials?
- How will we know if it’s working?
- How long will this take?
This is not about choosing between warmth and effectiveness. Good therapy should have both.
If you want support and space to reflect — that’s valid. If you want symptom relief and real change — that’s valid too. The key is that clients should be informed and empowered, not left guessing.
Therapy should feel supportive. But it should also move you forward.
We don’t accept subpar care for heart disease or diabetes. We shouldn’t accept it for mental health either. We are capable of expecting more. Of learning more. Of doing better.
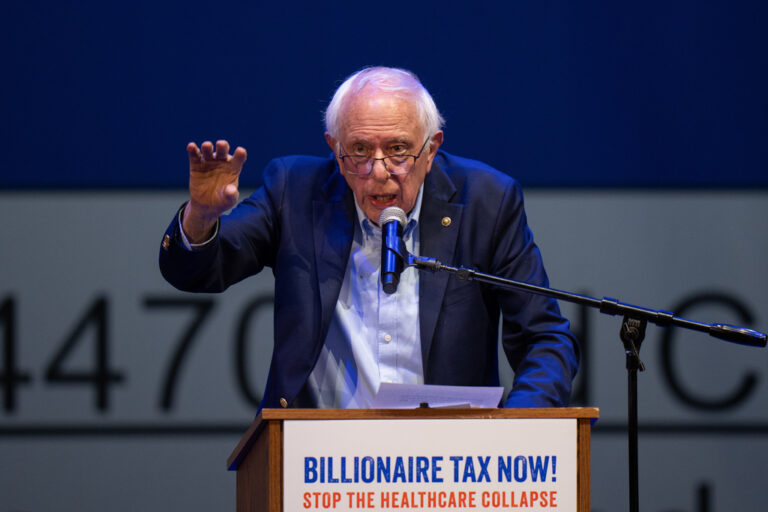
That’s why, as part of our mission to increase access to effective care, The CBT/DBT Center is hosting a FREE, virtual event: The Therapy Should Work Event, now until May 15.
This five-day event is an educational opportunity for the frum community to upgrade its understanding of what effective mental health care looks like. It features interviews with over 30 of the world’s leading experts — including the developers of CBT, PE, ERP, CPT, DBT, and more. These are the people who designed the protocols and trained the field.
Whether you’re in therapy, considering therapy, supporting a loved one, or simply want to understand how real healing happens, this summit is for you.
To register FREE or learn more, visit www.therapyshouldwork.com/










11 Responses
All licensed therapists practice CBT/ERP & beyond & all have a large number of clients who remain with symptoms. Therapy only has about a 41% success rate with depression according to the NIH, & for anxiety 51%.
Depression & anxiety are difficult illnesses to treat & for many people are a chronic struggle no matter how skilled the therapist is.
While short-term therapies like CBT and ERP can help with specific symptoms, especially when the problem is clear and focused (like a phobia or OCD), many people need more time for real and lasting change.
One large study looked at over 10,000 people in therapy and found that real improvement usually takes longer than we think. On average, people started seeing noticeable progress after about 20 sessions. But three out of four people didn’t really feel better enough until around 40 sessions—that’s about a year of weekly therapy. (This study is discussed in detail here: Psychiatry & Psychotherapy Podcast).
Also, a review published in the American Psychologist found that therapy effects from deeper, longer-term approaches often continue to grow after therapy ends—while the benefits from short-term approaches like CBT may fade more quickly. That’s because CBT often focuses on managing symptoms, rather than exploring the roots of emotional struggles. (See the full article here).
So while short-term therapy has its uses, the idea that deep emotional healing can usually happen in just 10–15 sessions isn’t backed by research. For many people, lasting change takes time, patience, and the space to explore their inner world more deeply.
Is this a paid advertisement?
The shade being thrown here is absolutely unnecessary for your marketing program.
Knock it off.Just about every therapist I know (and I know a lot of therapists), specializes in at least one evidence based therapy modality (and for the record, your list is far from complete).
As a fellow psychotherapist with considerable experience, I’m concerned that a well-intentioned article might inadvertently cause harm.
This article oversimplifies the concept of evidence-based practices, mistakenly labeling them as such when they should rather be described as manual-based treatments.
While some therapies do follow structured guides, many effective methods don’t, yet they are undeniably evidence-based.
Additionally, the duration of therapy isn’t just about cost or inconvenience; deeper, meaningful change often requires more extended treatment.
The focus of an article such as this should be on finding therapists who are ethical, skilled, and committed to ongoing improvement, rather than simply seeking shorter-term manual-based therapies.
This is only half the story. Take dbt for example. It targets self regulation. But what caused the self regulation? Getting to the core of the issue takes the most amount of time. Working through the traumas with IFS, EMDR, which are also evidence based.
This article, including the title “What our community deserves to know”, is deceiving and slightly manipulative. All of the modalities mentioned in this article are CBT based. Indeed CBT is more structured and concise, but it doesn’t work well for everyone and often doesn’t have long-lasting effects.
There are plenty of other psychotherapeutic approaches out there which are also evidence-based. Each issue and every client should be helped with a suitable strategy. CBT and its derivatives are good for certain challenges and for certain people.
Do your own research and choose the type of therapy that you feel speaks to you and the type of therapist that you will likely connect to.
Maybe don’t cause problems in the first place such as in school, when children are helpless against forced, bad therapy just because a child is not a rigid stereotype of a girl or boy. Like how I was forced to talk for the sake of talking because that is what girls do. Years of nitpicking by my parents and I attempted to be a yenta because that is what all women should be, getting fired from one job, losing an internship placement and nearly losing another job until I turned it around and did the complete opposite of the forced therapy. Now everything is working out nut I am deep in resentment at this overrated industry called therapy that everyone loves but I deeply hate. I can’t even be helped by therapy anymore since I have a deep, seething hatred of it. Therapists ask for too much money for therapy and if it does not work all I get is, go to another therapist. Just to pay again. Why does therapy get to hide behind that phrase but a doctor who ruins a person’s life will be sued for malpractice and cannot hide behind “try another doctor?”
Shame on you for either not understanding basic research in your own field or—worse—for understanding it and misusing it for self-promotion. If you want to tote EBP, go for it. But to attempt to throw under the bus good therapies and good therapists in our community because you are desperately trying to promote your preferred way has no place in the community. This is fear-mongering at its best and it only cheapens your professionalism in the eyes of your colleagues.
It is the official scientific conclusion of the American Psychological Association, based on a comprehensive review of psychotherapy research by a blue-ribbon expert panel, that ” evidence-based” practices DO NOT YIELD ANY SPECIAL BENEFITS OVER TREATMENT AS NORMAL.
Look it up for yourself.
For those clients and therapists out there that are still pursuing REAL therapy- don’t let this get you down. Heal the world.
This article is scientifically incorrect. The research demonstrates the exact opposite. Check out Jonathan Shedler’s work on this topic. Below is an excellent sampling of his work on this exact topic:
https://www.mcleanhospital.org/video/lecture-examining-evidence-evidence-based-therapy
In the end of the day, nothing replaces real therapy. Gotta do the work…
I am a trained, practicing therapist.
I am also a therapy client / patient.
I have been to residential in-patient treatment.
I have personally talked with thousands (!) of people with mental health struggles.
This article is incorrect, misleading and dangerous.
It is also, whether intentionally or not, paid or not, an advertisement. And since the service/offering is free, that means we, you and me reading this, are the PRODUCT.
Will you sell out and buy in?